Stevens-Johnson syndrome is generally considered to be a medication-induced condition. However, cases of non-drug-related SJS also occur, particularly related to hair dye containing paraphenylene diamine (PPD).
Even when hair dye is used properly, it can still cause toxicity, including skin damage and severe allergic reactions. Permanent hair dyes are most frequently associated with health risks because they contain a variety of strong chemicals, including ammonia, hydrogen peroxide, resorcinol, and PPD.
What is PPD?
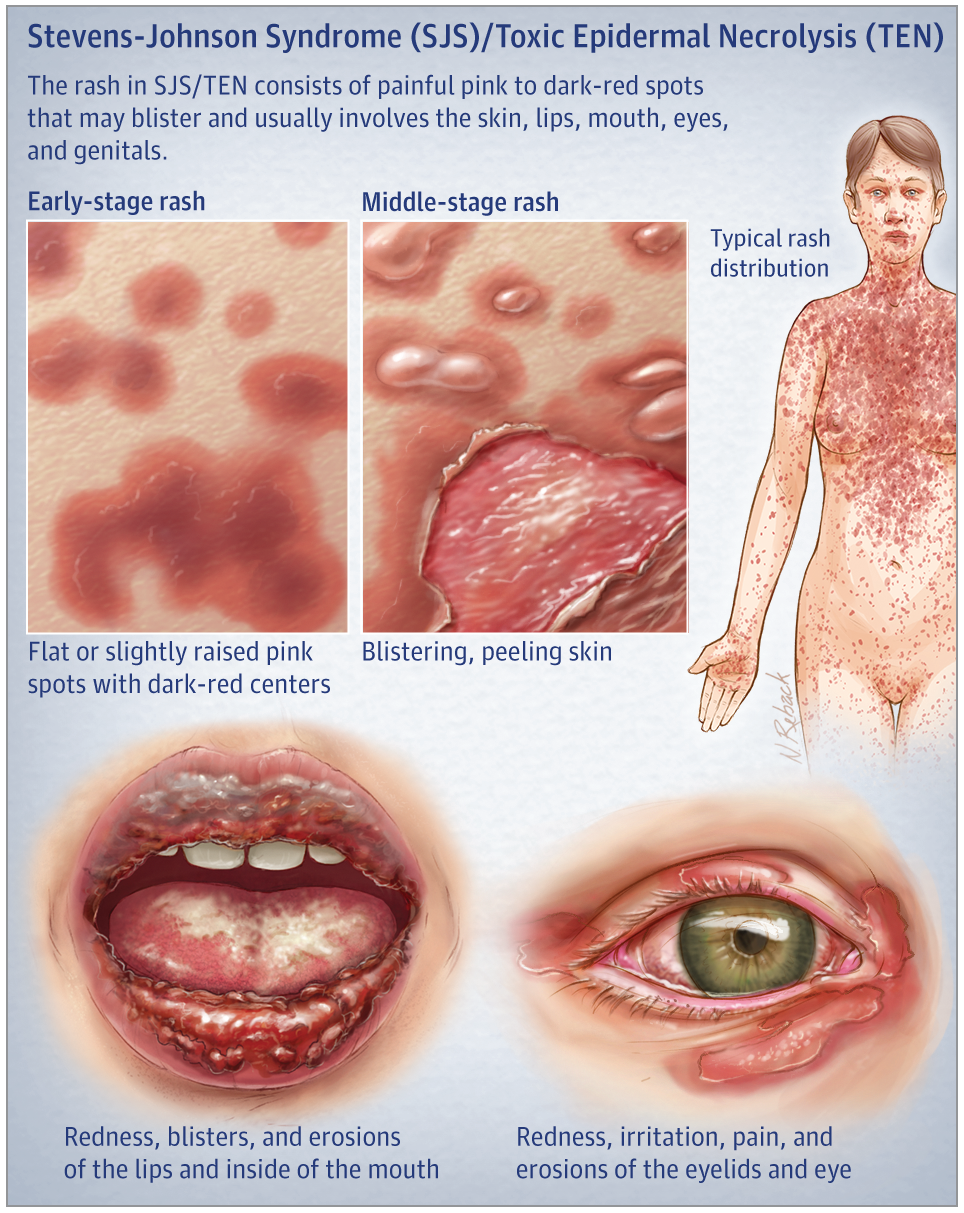
PPD is a frequent component of permanent hair dye products and temporary henna tattoos, and exposure to it has been proven to cause severe facial edema, redness, sores, itching, burning, and contact dermatitis followed by erythema multiforme (EM) a form of SJS in sensitized patients. Other chemicals suspected to cause EM include bromofluorene, colophony, fragrances, epichlorohydrin, 1,2-ethanedithiole, and epoxy resin.
An allergic reaction to hair dye is an important health concern in connection with Stevens-Johnson syndrome because many people continue to use the dye in spite of an obvious allergy to it, putting them at risk for SJS. Although many hair dyes are marketed as non-allergenic or PPD-free, these products often contain cross-reactive chemicals such as toluene-2,5-diamine sulfate, which nearly 50 percent of those allergic to PPD are also allergic to.
Because of this cross-reactivity, dermatologists often recommend that patients allergic to PPD not use permanent hair dye, but patients are often unwilling to follow this advice and instead continue coloring their hair and tolerating the itching and rash that commonly follows. Although a patch test is typically required before applying hair dye, most people at home and in salons do not perform this test, believing that because no complication occurred during the last application, no adverse reaction will happen this time either.
Other Stevens-Johnson Syndrome News
A study has found that survivors of Stevens-Johnson syndrome (SJS) have a higher risk of cardiovascular problems, specifically cerebrovascular accidents and ischemic heart disease, compared to the general population.
Medical negligence may contribute to Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). Learn how drug errors, misdiagnosis, or lack of warnings could support a legal claim.
Lamictal has been linked to Stevens-Johnson Syndrome (SJS), a life-threatening skin reaction. Learn how improper prescribing or dosing may lead to serious injuries and legal action.
If you've been diagnosed with Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis, it’s critical to act quickly and consult an experienced attorney to protect your legal rights and potential claim.
Allopurinol, a common gout medication, has been linked to Stevens-Johnson Syndrome—a rare but serious skin reaction that may require hospitalization and lead to long-term complications.
Improperly prescribed Allopurinol and Lamictal are leading causes of SJS/TEN. Learn how medical errors may have contributed to your injury—and why early legal action is essential.